Abstract:
Researchers at Kanazawa University report in Nature Communications the mechanism making some lung-cancer patients resistant to the drug osimertinib. In addition, they suggest a combined drug treatment resolving osimertinib resistance in the case of cancer cells expressing low amounts of AXL, a protein belonging to the class of receptor tyrosine kinases.
The effectiveness of cancer treatment is often hampered by cancer cells being heterogeneous. This is the case for EGFR-mutated lung cancer: drugs based on biomolecules of a type known as tyrosine kinase inhibitor (TKI) have been used to treat the disease, but with various levels of efficacy. (EGFR stands for “epidermal growth factor receptor”, a protein playing an important role in signaling processes from the extracellular environment to a cell.) Sometimes, tumor cells are simply resistant to the drug. Now, Seiji Yano from Kanazawa University and colleagues have investigated the efficacy of the TKI osimertinib for treating EGFR-mutated lung cancer, and how it relates to the expression in tumor cells of a particular protein called AXL. They found that both AXL-high and -low expressing tumor cells showed tolerance (acquired resistance) to osimertinib, but that the mechanisms involved are different for the two situations. Moreover, the researchers suggest a way to enhance the success of osimertinib treatment for the case of AXL-low expressing tumors.
First, the scientists compared the susceptibility to osimertinib in both AXL-high and -low expressing tumor cells in in vitro experiments. They observed that osimertinib inhibited the viability of the cancer cells in both cases, but that the sensitivity to the drug was higher for AXL-low expressing EGFR-mutated lung cancer cells. They also noticed that a small number of tumor cells survived the procedure — an indication of osimertinib tolerance. These findings were consistent with results from the clinical study of the drug performed earlier on 29 patients with EGFR-mutated non-small cell lung cancer.
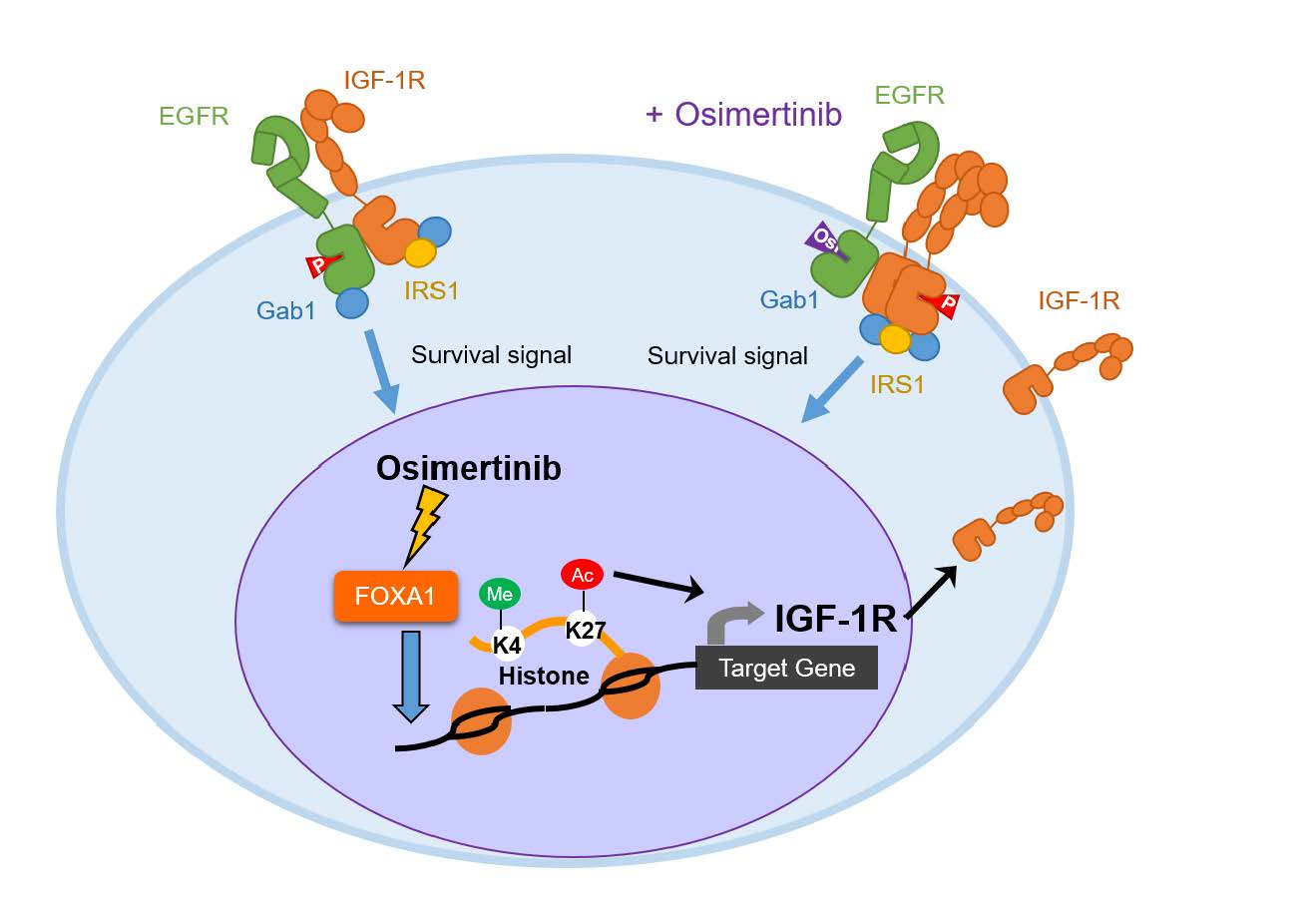
Through experiments aiming to understand the mechanism behind osimertinib tolerance, Yano and colleagues discovered that phosphorylation of IGF-1R was increased in AXL-low-expressing tumor cell lines, but not in AXL-high expressing tumors. (IGF-1R stands for ‘insulin-like growth factor 1 receptor’; it is a protein located on the surface of human cells. Phosphorylation is the chemical process of adding a phosphoryl group.) The researchers then found that phosphorylated IGF-1R supported the survival of AXL-low expressing tumors after exposure to osimertinib.
The scientists then tested whether the observed osimertinib resistance could be resolved by administering linsitinib, a substance known to inhibit the phosphorylation of IGF-1R. Encouraged by the positive outcome of the experiment, Yano and colleagues went further and evaluated the combination of osimertinib and linsitinib. Their conclusion was that the transient combination of linsitinib with continuous osimertinib treatment could cure or at least dramatically delay tumor recurrence in AXL-low-expressing EGFR-mutated lung cancer. More investigating needs to be done, though. Quoting the researchers: “… the safety and efficacy of the transient combination of IGF-1R inhibitor and osimertinib should be evaluated in the clinical trials.”
Figure
Mechanism of targeted drugs tolerance in lung cancer cells
[Background]
Tyrosine kinase inhibitors
A tyrosine kinase inhibitor is a drug inhibiting (that is, preventing or reducing the activity of) a specific tyrosine kinase. A tyrosine kinase is a protein (enzyme) involved in the activation of other proteins by signaling cascades. The activation happens by the addition of a phosphate group to the protein (phosphorylation); it is this step that a tyrosine kinase inhibitor inhibits. Tyrosine kinase inhibitors are used as anticancer drugs. One such drug is osimertinib, used to treat EGFR-mutated lung cancer.
AXL
AXL is a receptor tyrosine kinase — a tyrosine kinase consisting of an extracellular part, a transmembrane part (‘sitting’ within a cell membrane) and an intracellular part. AXL regulates various important cellular processes, including proliferation, survival and motility. In recent years, it has become clear that AXL is a key facilitator of drug tolerance by cancer cells. Seiji Yano from Kanazawa University and colleagues have found that this is also the case for EGFR-mutated lung cancer. While a high expression of AXL correlates with resistance to osimertinib, such tolerance also occurs in AXL-low-expressing cancer cells. Yano and colleagues have now found that for the latter case, phosphorylation of IGF-1R (insulin-like growth factor 1 receptor) is responsible for the resistance to osimertinib.
Article
Transient IGF-1R inhibition combined with osimertinib eradicates AXL-low expressing EGFR mutated lung cancer
Journal: Nature Communications
Authors: Rong Wang, Tadaaki Yamada, Kenji Kita, Hirokazu Taniguchi, Sachiko Arai, Koji Fukuda, Minoru Terashima, Akihiko Ishimura, Akihiro Nishiyama, Azusa Tanimoto, Shinji Takeuchi, Koshiro Ohtsubo, Kaname Yamashita, Tomoyoshi Yamano, Akihiro Yoshimura, Koichi Takayama, Kyoichi Kaira, Yoshihiko Taniguchi, Shinji Atagi, Hisanori Uehara, Rikinari Hanayama, Isao Matsumoto, Xujun Han, Kunio Matsumoto, Wei Wang, Takeshi Suzuki, Seiji Yano
DOI: 10.1038/s41467-020-18442-4
Funder
This work was supported by JSPS KAKENHI Grant Number JP16H05308, the Project for Cancer Research And Therapeutic Evolution (P-CREATE) from the Japan Agency for Medical Research and development, AMED, Grant Number 16cm0106513h0001, research grants from Boehringer-Ingelheim, Eisai, and MSD, and Extramural Collaborative Research Grant of Cancer Research Institute, Kanazawa University.



 PAGE TOP
PAGE TOP