Abstract:
Recent epidemiological studies dispute a widely held belief that patients with type 2 diabetes develop renal decline accompanied by overt proteinuria. However, little is known about renal prognosis and mortality in patients who develop renal decline without proteinuria. Using a propensity score matching technique, this study revealed that renal prognosis and all-cause mortality were better among those without proteinuria, compared with those with proteinuria. These findings suggest that proteinuria is an important prognostic factor in patients with type 2 diabetes and renal decline.
[Background]
Recent reports showed that in Japan, there are about 10 million diabetic patients. Among these, 25-40% are expected to develop diabetic kidney disease in their lifetime. Based on epidemiological studies, primarily in type 1 diabetes, it has been considered that the clinical course of diabetic kidney disease starts from (1) normoalbuminuria to (2) microalbuminuria, to (3) macroalbuminuria (proteinuria), to (4) renal decline, and finally to (5) hemodialysis. In addition, it has been considered that renal biopsy of diabetic patients with renal decline shows typical glomerular lesions, represented by nodular glomerular sclerosis*1). Recent cross-sectional studies, however, revealed that about 40% of patients with type 2 diabetes develop renal decline without proteinuria. However, clinicopathological characteristics, renal prognosis, and all-cause mortality in patients with renal decline without proteinuria are scarce.
[Results]
On behalf of the Research Group of Diabetic Nephropathy, the Ministry of Health, Labour and Welfare and the Japan Agency for Medical Research and Development, T. Wada and his research team from Kanazawa University, conducted a comprehensive study of the renal biopsy registry. Renal biopsies were performed at 18 hospitals in Japan from January 1985 through December 2016. 526 patients were studied, who had an eGFR*2) value, an index of renal function, of <60 mL/min/1.73m2 at the time of biopsy. Among them, 88 patients did not have proteinuria (urine albumin-to-creatinine ratio, ≥300 mg/g), while 438 patients had proteinuria. For comparative analyses, a statistical method called propensity score matching*3), addressing the imbalance of age, sex, diabetes duration, and eGFR at the time of biopsy, was used. As a result, 82 patients without proteinuria was compared with 164 patients with proteinuria.
Those without proteinuria had a lower systolic blood pressure compared with those with proteinuria, although the use of renin-angiotensin blockade was lower in those without proteinuria. Renal histopathology revealed that those without proteinuria had mild glomerular changes (62%), while those with proteinuria showed typical glomerular diabetic changes known as nodular lesions (66%). Those without proteinuria showed less severe tubulointerstitial lesions*4) and arteriolar lesions*5).
The progression of chronic kidney disease (either (1) end-stage renal disease (commencement of hemodialysis, peritoneal dialysis, kidney transplantation, or kidney disease-related death), (2) decrease of eGFR by ≥50%, or (3) doubling of serum creatinine) and all-cause mortality were better in those without proteinuria, compared in those with proteinuria (Figure 1).
[Future prospects]
This study suggests that proteinuria is an important prognostic factor in patients with type 2 diabetes and renal decline. Further studies on mechanisms of not developing proteinuria and kidney protection are needed.
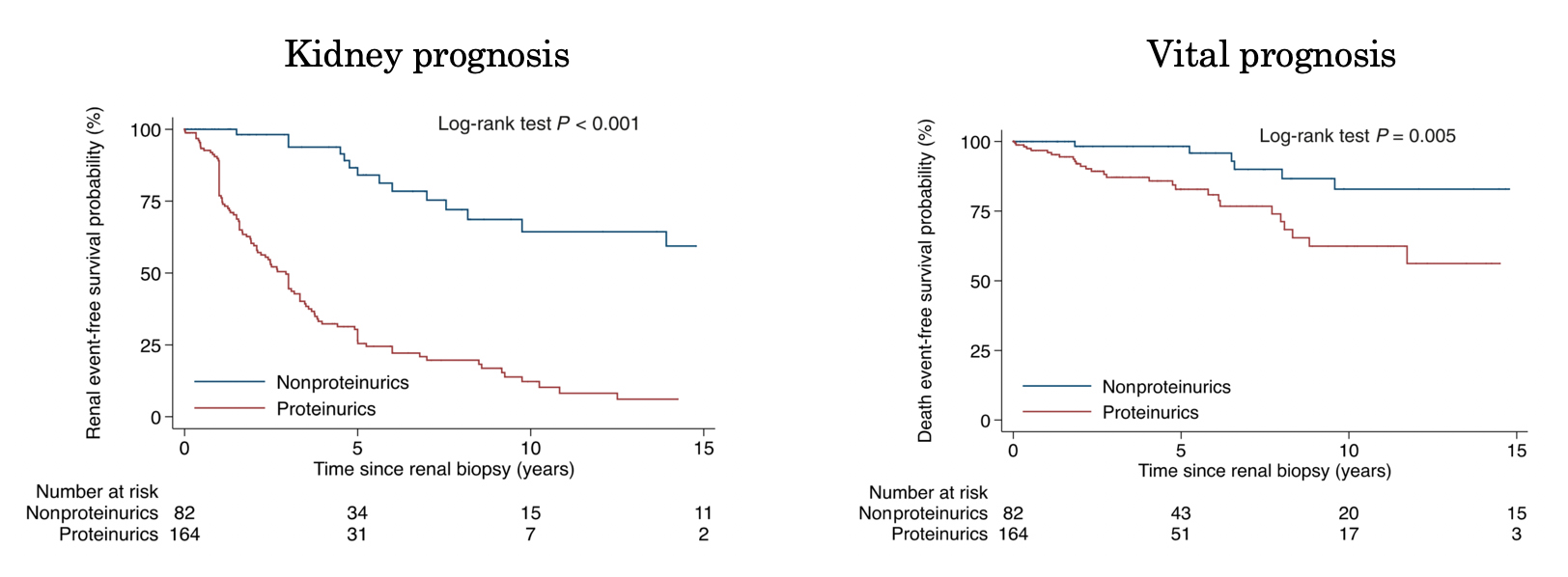
Figure.
Kidney prognosis and vital prognosis of nonproteinuria cohort and proteinuria cohort. Kaplan-Meier curves*6) were calculated based on follow-ups, taking time 0 as the date of renal biopsy. Kidney prognosis: Kaplan-Meier curves of the patients, after propensity score matching, who did not have renal events. After a median follow-up of 1.9 years from the date of renal biopsy, 124 of the 246 matched patients had renal events. The 5-year chronic kidney disease progression-free survival was 46.4% for all patients, 86.6%for the nonproteinuric diabetic kidney disease cohort, and 30.3% for the proteinuric diabetic kidney disease cohort. Vital prognosis: Kaplan-Meier curves of the propensity score matched cohort. After a median follow-up of 3.1 years from the date of renal biopsy, 35 of the 246 matched patients had death events. The 5-year death-free survival was 88.2% for all patients, 98.3% for the nonproteinuric diabetic kidney disease cohort, and 82.6% for the proteinuric diabetic kidney disease cohort.
[Glossary]
*1) Nodular lesion
Acidophilic substances precipitate on nodules in mesangial substrates and cellular components locate in the periphery of the mesangial region. Most characteristic pathology in diabetic kidney disease.
*2) eGFR
Estimated glomerular filtration rate. eGFR is calculated from serum creatinine, age and sex. eGFR less than 60 mL/min/1.73 m2 indicates moderate or more renal decline.
*3) Propensity score matching
A technique used in statistical analyses, introduced by Rosenbaum and Rubin in 1983. In various studies, the background of subjects in a group of interest is often different from that of a comparison group. Propensity score matching is one of the techniques to reduce the influence of different background factors.
*4) Tubulointerstitial lesion
Renal tubules play important roles in reabsorbing necessary components such as electrolytes and water from the glomerular filtrate and in returning them into the blood, excreting unnecessary components into the urine. The tissue between renal tubules is the interstitium, and a disorder of the interstitium is called the tubulointerstitial lesion. Tubulointerstitial lesion is found in many kidney disorders with no abnormalities in urine tests, whose causes are unknown. Tubulointerstitial lesion should be suspected in such cases.
*5) Arteriolar lesion
Arteriolar lesion is caused by a narrowing of the inner diameter of arterioles in the case of continuing high blood pressure, which exerts extra pressure on arterioles serving the glomeruli and induces proliferation of arteriolar epithelial cells. Upon reduction of blood flow in glomeruli where much blood flow is necessary, glomerular sclerosis gradually progresses and renal functions decrease, which may lead to chronic renal failure.
*6) Kaplan-Meier curve
Kaplan-Meier curve indicates a graph showing events occurring in the group of research interest. The ordinate indicates the ratio of subjects that have not yet had an event and at time zero, it is 100%. The abscissa indicates the lapse of time. In medical research, with time lapse, more events take place (the ratio of subjects not having had an event decreases), making the Kaplan-Meier curve decrease. Depending on characteristics of a group of interest (for example, proteinuria cohort and nonproteinuria cohort), the extent of decrease could be analyzed by statistical methods, survival analysis, such as log-rank test.
Article
Nonproteinuric versus proteinuric phenotypes in diabetic kidney disease: a propensity score-matched analysis of a nationwide, biopsy-based cohort study
Journal: Diabetes care
Authors: Masayuki Yamanouchi, Kengo Furuichi, Junichi Hoshino, Tadashi Toyama, Akinori Hara, Miho Shimizu, Keiichi Kinowaki, Takeshi Fujii, Kenichi Ohashi, Yukio Yuzawa, Hiroshi Kitamura, Yoshiki Suzuki, Hiroshi Sato, Noriko Uesugi, Satoshi Hisano, Yoshihiko Ueda, Shinichi Nishi, Hitoshi Yokoyama, Tomoya Nishino, Kenichi Samejima, Kentaro Kohagura, Yugo Shibagaki, Koki Mise, Hirofumi Makino, Seiichi Matsuo, Yoshifumi Ubara, Takashi Wada, and Research Group of Diabetic Nephropathy, the Ministry of Health, Labour and Welfare, and the Japan Agency for Medical Research and Development
DOI: 10.2337/dc18-1320
Funder
This study was supported in part by a Ministry of Health, Labour and Welfare Grant-in-Aid for Diabetic Nephropathy and Nephrosclerosis Research (JP17ek0310003).



 PAGE TOP
PAGE TOP