Abstract:Researchers at Kanazawa University have shown that a combination of innovative immunomodulation with traditional chemotherapy may prove efficacious in combatting advanced cancer of the pancreas. In an experimental mouse model of pancreatic ductular adenocarcinoma, they showed that the nucleoside analog gemcitabine combined with anti-PD-1 antibody-based immunotherapy (targeting immune checkpoint protection exploited by cancer cells) has the potential to improve outcomes in selected patients of intractable pancreatic cancer with metastases.
Kanazawa, Japan – Bertolt Brecht, the German playwright, famously said, “Mixing one's wines may be a mistake, but old and new wisdom mix admirably.” Now, researchers at Kanazawa University have shown that a combination of innovative immunomodulation with traditional chemotherapy may prove efficacious in combatting metastatic cancer of the pancreas.
Pancreatic cancer is a dreaded malignancy, the commonest variant being pancreatic ductular adenocarcinoma (PDAC). Most patients present in advanced stages, with only about a fifth amenable to curative surgery at diagnosis. Conventional chemotherapy involves the drug Gemcitabine (GEM) but, unfortunately, the outcome is often bleak.
The research team had previously elucidated the association of human PDAC with local and systemic immune responses. Now, they have speculated about immunomodulation as a novel alternate or adjuvant treatment strategy. Immune checkpoints moderate the immune system by precluding indiscriminate attacks. Programmed cell Death 1 (PD-1) is a checkpoint protein present on immune cells (T lymphocytes) that functions as a ‘brake’ or ‘off-switch’ when bound to ligands such as PD-L1. Some cancer cells have abundant PD-L1 which camouflages them from immune attack; antibodies targeting PD-1 or PD-L1 can circumvent this subterfuge. Immune Checkpoint Inhibitors are being evaluated for treating certain cancers.
Lead author Tuyen Thuy Bich Ho explains the research protocol. “We established a model of PDAC by injecting a murine pancreatic cancer cell-line into the spleens of experimental mice. They were then treated with anti-PD-1 antibody, GEM, or a combination of both, and evaluated against a control group receiving no treatment. We assessed liver metastases, immune cell infiltration, gene expression, immune cell response phenotypes, and overall survival.”
The results unequivocally favored the combination protocol. Mice treated with combined immunotherapy and chemotherapy survived the longest. Their metastatic tissues showed increased Th1 lymphocyte and M1 macrophage infiltration. The gene expression profile of peripheral blood cells highlighted T cell and innate immune signaling pathways suggesting that immune checkpoint inhibition had reduced the PD-1-mediated cancer protection. Additionally, expanded lymphocytes drawn from the spleen showed increased M1 macrophages signifying classically activated anticancer immunity.
“Our findings indicate that immunomodulation with anti-PD-1 antibodies may potentiate the action of gemcitabine against pancreatic cancer,” says corresponding author Dr Yoshio Sakai. “However, our results were obtained in an experimental murine model and there are significant disparities in the immune characteristics and therapeutic responses of human disease. Therefore, we recommend further investigation to clarify the role and applicability of this encouraging combination in the management of intractable pancreatic cancer.”
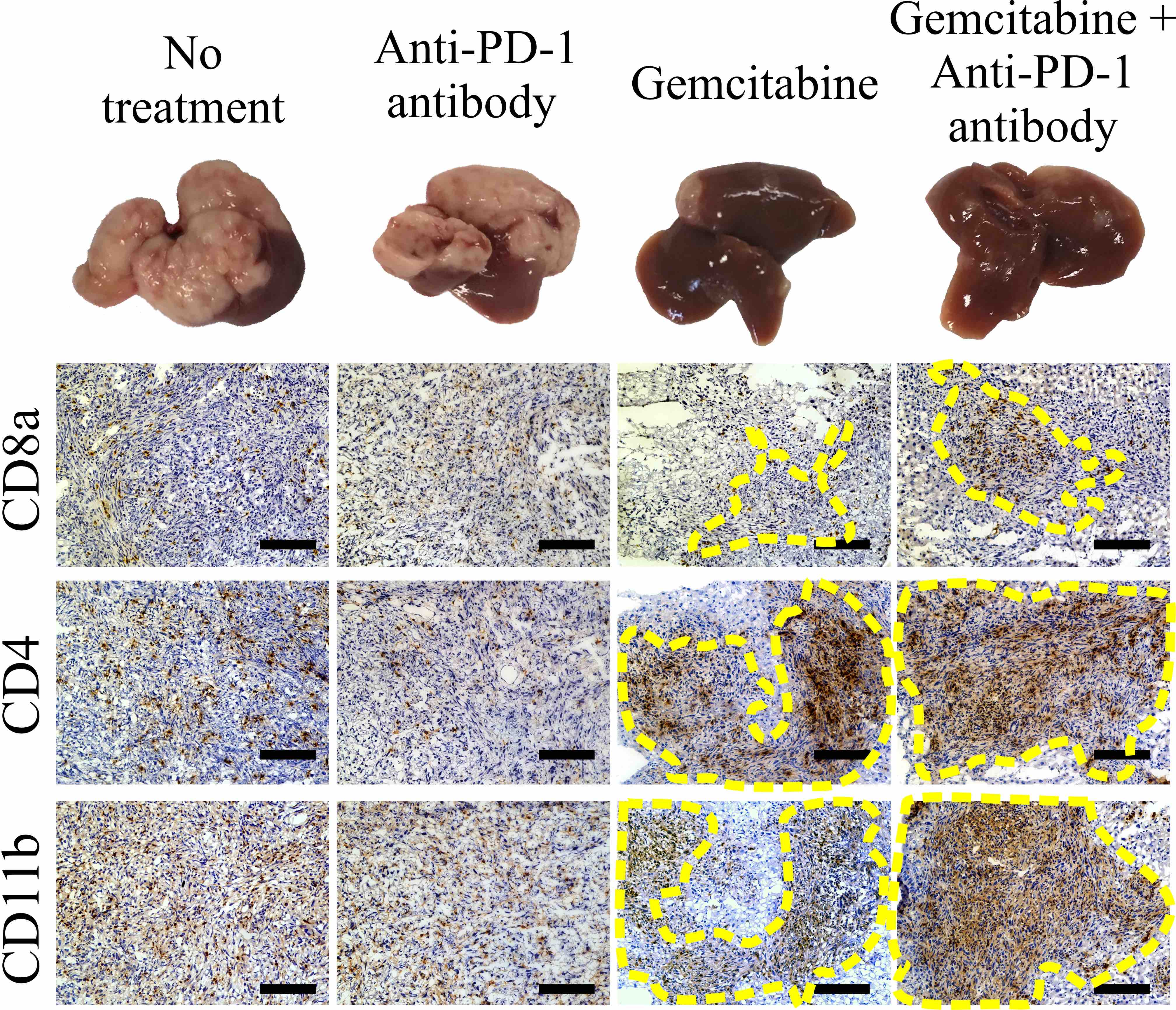
figure1
Histological findings of the immune-response induced by combination therapy of Gemcitabine and anti-PD-1 antibody.
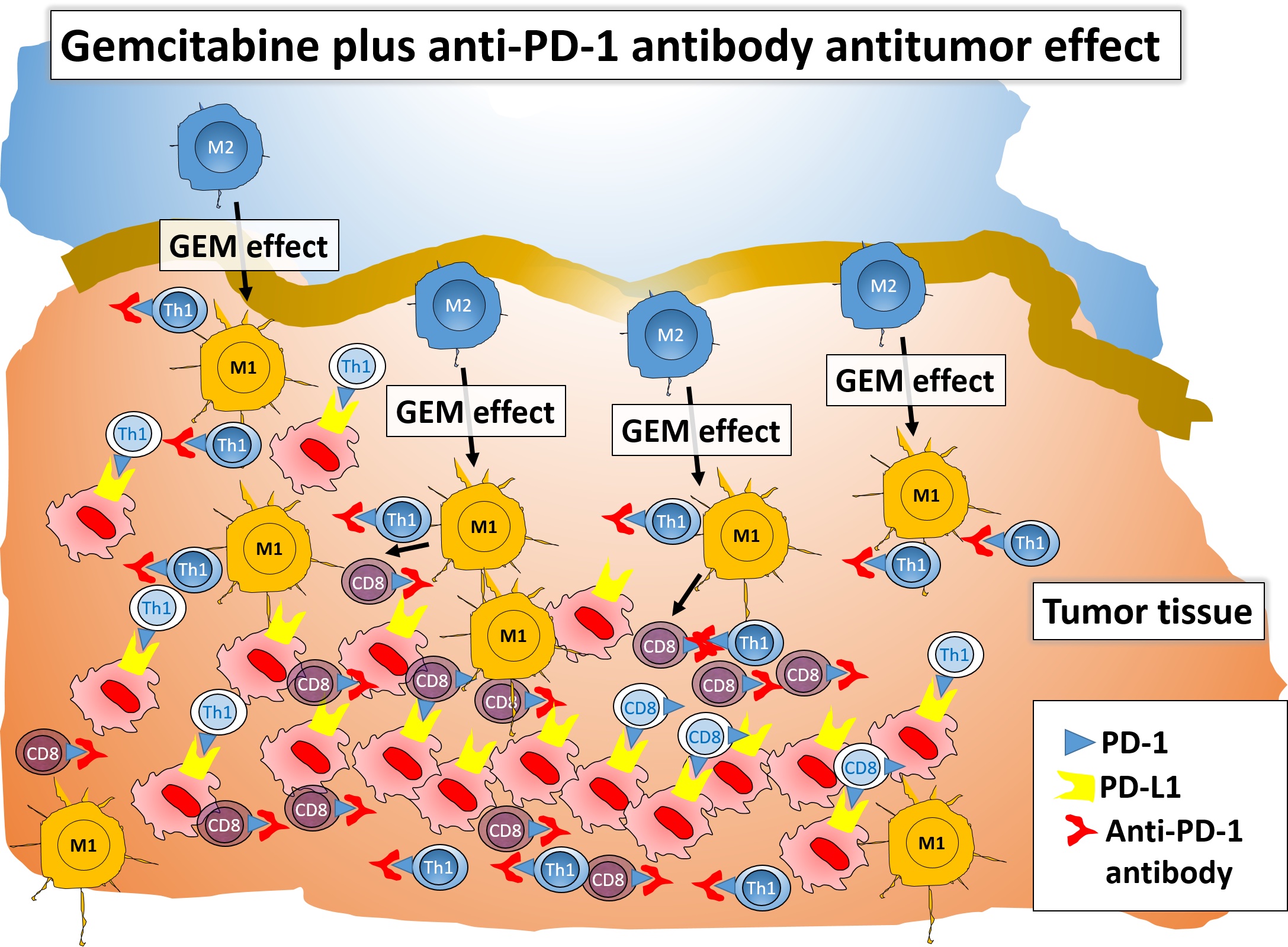
figure2
Overview of the Gemcitabine plus anti-PD-1 effect. The combination of Gemcitabine and anti- PD-1 antibody is an effective chemo-immunotherapy for a murine model of PDAC liver metastasis. We confirmed that the antitumor response is enhanced by mediation of CD4+ Th1 lymphocytes and M1-type macrophages, furthermore, the effect is associated with an increased activity of CD8+ T cells.
[Article]
Title:Combination of gemcitabine and anti-PD-1 antibody enhances the anticancer effect of M1 macrophages and the Th1 response in a murine model of pancreatic cancer liver metastasis
Journal: Journal for Immunotherapy of Cancer
Authors:Tuyen Thuy Bich Ho, Alessandro Nasti, Akihiro Seki, Takuya Komura, Hiiro Inui, Takashi Kozaka, Yoji Kitamura, Kazuhiro Shiba, Taro Yamashita, Tatsuya Yamashita, Eishiro Mizukoshi, Kazunori Kawaguchi, Takashi Wada, Masao Honda, Shuichi Kaneko, Yoshio Sakai
[Funder]This work was supported in part by a subsidy from the Japanese Ministry of Education, Culture, Sports, Science, and Technology.



 PAGE TOP
PAGE TOP